Technical assistance, quality assessment, and other support for the implementation of Primary Care First
Objective
Supported the Centers for Medicare & Medicaid Services and approximately 3,000 practices nationwide to implement Primary Care First, a value-based care model designed to improve the health of millions of Medicare beneficiaries while reducing health care costs.
Approach
We provided technical assistance, practice management, payment calculations, quality assessment, and policy analysis to facilitate Primary Care First implementation and operations.
Impact
Primary Care First implementation and operations activities are helping participating clinicians reduce health care costs while ensuring quality of care is maintained. Lessons learned from implementing the model will inform future strategies and policies related to value-based care.
What is primary care?
The Institute of Medicine defines primary care as, “the provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community.”
Primary care is linked to improved health outcomes and health care quality, including:
- Lower mortality rates
- Lower rates of hospital and emergency department utilization
- Better self-rated health
- Higher patient satisfaction with care
- Greater receipt of recommended preventive care services
The Impact of Primary Care on Population Health
Importantly, in geographic areas or health care systems with a strong primary care infrastructure, these positive outcomes are more evenly distributed among population subgroups. Primary care is also consistently associated with lower use of health care resources and lower total cost of care. Thus, primary care effectively advances the “triple aim” of health care—better population health and experiences of care at lower cost.
Improving Primary Care in the U.S.
Despite its demonstrated value, primary care has been chronically underfunded in the United States. Within Medicare, primary care spending accounts for only 2-5% of total spending among fee-for-service beneficiaries. In contrast, the average primary care spending rate among other Organization for Economic Cooperation and Development countries is over 12%.
Recent efforts to revitalize the primary care system in the U.S. have championed the patient-centered medical home (PCMH) as a path forward. This model of primary care organization, delivery, and funding embodies health care that is:
- Patient-centered
- Comprehensive
- Coordinated
- Accessible
- Committed to quality and safety
Results from evaluations of PCMH demonstrations have shown small positive impacts on health outcomes, patient experiences of care, and receipt of preventive care services. However, large positive impacts remain elusive, presumably because the current fee-for-service (FFS) payment structure inadequately supports the changes in delivery system infrastructure, staffing, and workflows necessary to implement and sustain a successful PCMH model.
Patient-Centered Medical Homes as a Strategic Direction for Medicare
PCMH models accompanied by payment structures aligned with PCMH principles, are one strategic area of focus for the Centers for Medicare & Medicaid Services (CMS). The CMS Innovation Center (CMMI) was established in 2010 to test new health care payment and service delivery models, known as alternative payment models (APMs). The overarching goal of these APMs is to transition clinicians, health systems, and patients to a reimbursement system that pays for the value of care (e.g., quality, efficiency) rather than the volume of care delivered (i.e., traditional FFS payment structure). Transitioning to value-based care would consequently improve the health of millions of Medicare beneficiaries.
Transitioning to Value-Based Care with Primary Care First
Primary Care First, CMMI’s newest PCMH model, is geared towards advanced primary care practices that are prepared to move away from FFS into a partial capitation model that carries some financial risk. In return, practices have greater flexibility to comprehensively meet the needs of their complex, chronically ill patient population, while innovating to improve health and quality of care outcomes.
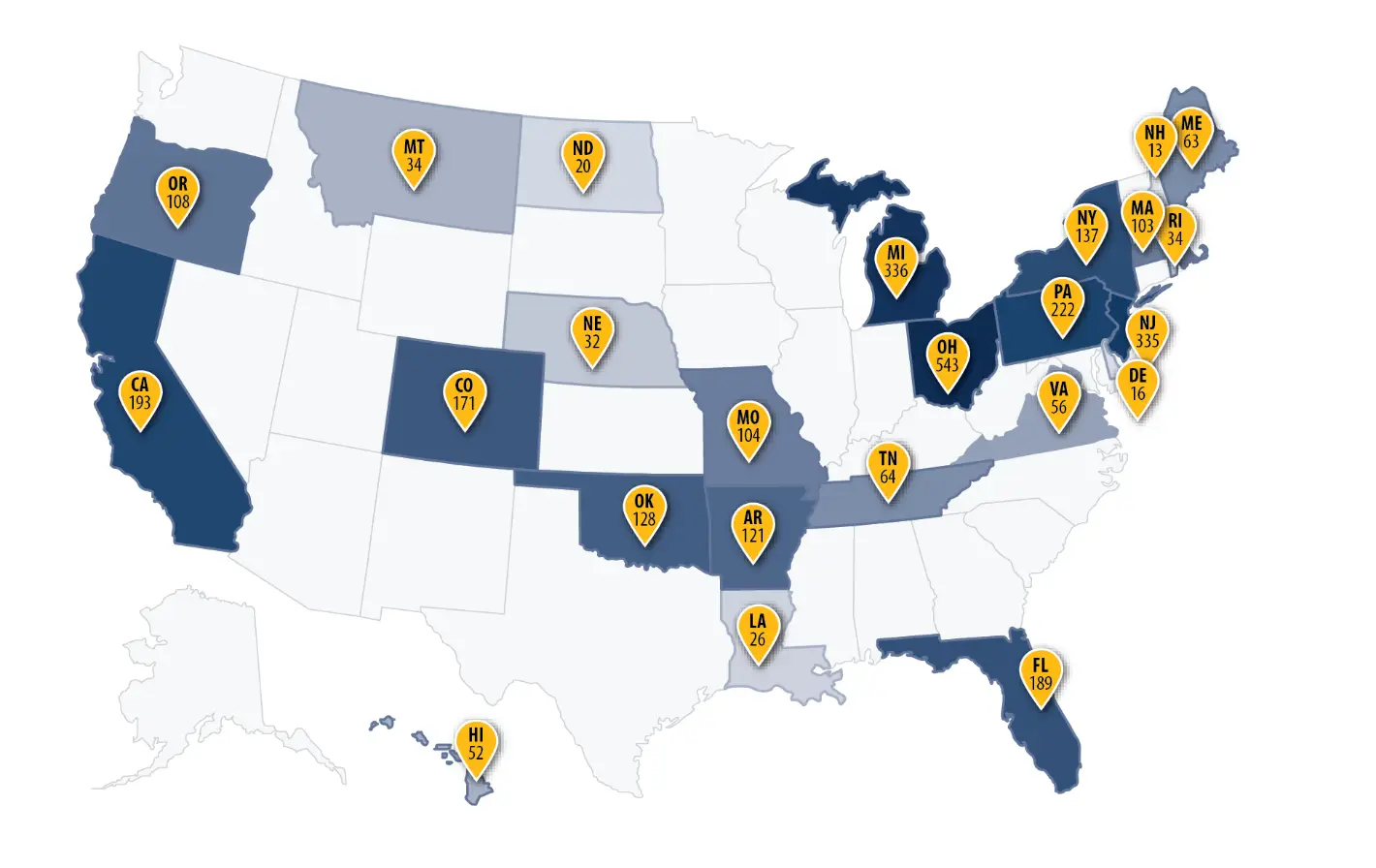
Rolled out in January 2021, Primary Care First currently includes 25 regions and approximately 800 practices across the country (see Figure 1) with an expected expansion to approximately 3,000 practices in 2022.
How Primary Care First Works
In Primary Care First, CMS provides payments to participating practices that are higher, in aggregate, than historical Medicare FFS payments, thus enabling these practices to provide care consistent with PCMH principles. Recognizing that aligning quality and value incentives across the entirety of a patient panel is paramount, Primary Care First is a multi-payer model that also includes 14 payer partners from commercial and state Medicaid plans.
RTI Provides Large-Scale Implementation Support and Analytic Resources
As a research institution with decades of organizational experience in Medicare policy, RTI International supports CMS in the implementation of the Primary Care First model through the following activities:
- Technical Assistance - Providing support to participating clinicians, practice teams, payer partners, and other external stakeholders
- Practice Management - Maintaining up to date practice practitioner information to sustain accurate beneficiary assignment and model payments
- Payment Calculation - Identifying the patients for whom participating practices are responsible for managing total costs and calculating model payments to practices
- Quality Assessment - Assessing the quality of care provided by participating practices using various quality of care measures
- Policy Analyses - Conducting analyses to inform the development of model policies related to practice monitoring, patient attribution, payment, and quality measurement
RTI International is proud to partner with CMS in the effort to invest in and transform the U.S. primary care system while serving a significant role in improving the human condition.
Figure 1. Number of Participating Practices by PCF Region
- Centers for Medicare & Medicaid Services (CMS)







