The COVID-19 pandemic is having a profound health and socioeconomic impact in more than 80 countries around the world, as governments enact lockdowns and quarantine measures, many people shift to working from home, schools shut down, and businesses shutter their doors, unsure of when and if they will be able to reopen. But for governments, especially their health institutions, this is no time to halt essential services.
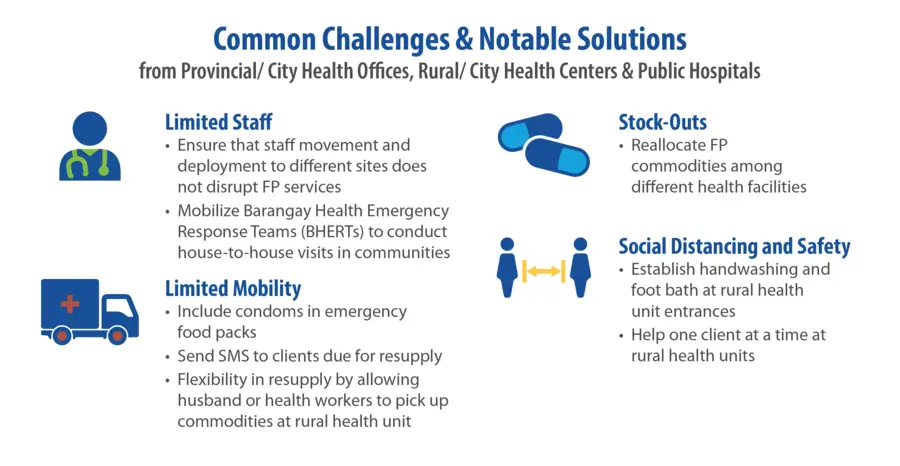
Instead, it is a time to ensure that these services are not interrupted. In the Philippines, the government has deemed family planning (FP) services as an essential health care service that must be continued in order to keep Filipinos safe during the pandemic. Two weeks into the lockdown of the Luzon group of islands, which are home to about half of the entire population of the Philippines, the Commission on Population and Development (POPCOM) and Department of Health (DOH) issued guidance calling for cooperation amongst health facilities, local government units (LGUs), and community volunteers in order to continue to provide FP and reproductive health services and commodities in the face of COVID-19.
Soon after the release of this guidance, the RTI-led USAID ReachHealth project, which works to strengthen and improve access to FP for Filipino families, swiftly developed a rapid survey to see if the health facilities and LGUs served under the project would be able to adhere to this guidance with most parts of the country under varying degrees of community quarantine.
It is important to leverage new methodologies for data gathering, existing connections with health institutions, and technology to inform evidence-based action as we continue to confront challenges in the health sector and beyond during COVID-19.” – Dr. Ophelia Mendoza, Monitoring, Evaluation, Research, Learning and Adapting (MERLA) Director for the USAID ReachHealth Project
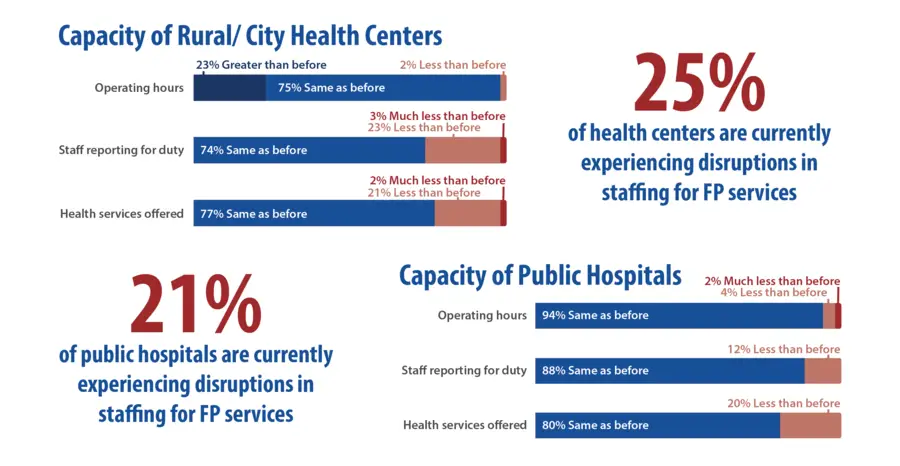
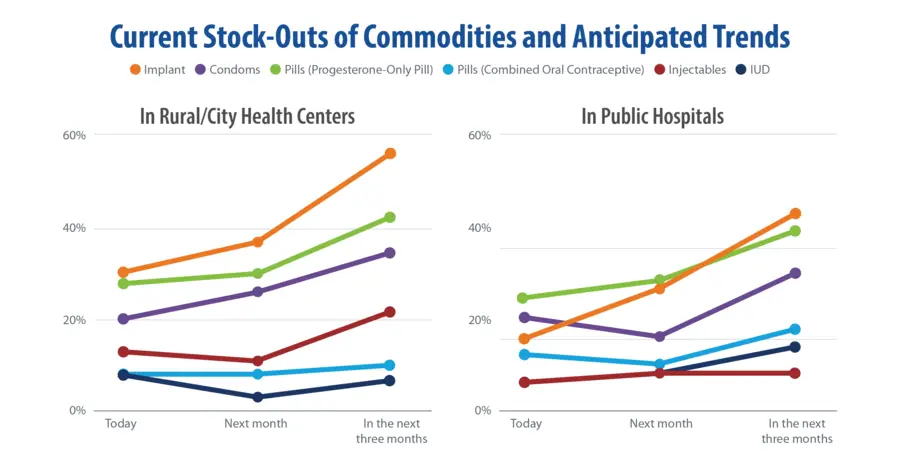
The project team carried out the rapid survey on March 31, 2020 by conducting phone interviews with FP coordinators and staff of rural and city health centers, public hospitals, and provincial and city health offices. Thanks to good relationships with local health facilities and governments, the project was able to interview more than 91% of target institutions across all 32 provinces and cities served by ReachHealth, collecting data from 29 provincial and city health offices, 175 health centers, and 57 public hospitals.