Avoiding unnecessary nursing facility resident hospitalizations can improve resident health, increase quality of care, and reduce health care costs
Objective
RTI evaluated a Centers for Medicare & Medicaid Services (CMS) initiative to improve nursing facility resident health, increase care quality, and lower Medicare expenditures by reducing the number of avoidable hospitalizations.
Approach
Using a mixed methods research design, we collected and analyzed data to determine the initiative effects on hospital utilization, Medicare expenditures, and care quality.
Impact
The clinical and education interventions (2012-2016) were associated with reductions in avoidable hospitalizations; the evaluation found no clear evidence that the payment incentive interventions (2016-2020) were associated with any favorable reductions in hospital use. The findings of the evaluation will help policymakers decide which interventions might be worth further investment.
Every year, about 25% of people who live in nursing facilities are transferred to hospitals for care. Although some of these transfers are required to treat specific health conditions or complications, many of these hospitalizations may be avoided through quick diagnosis and treatment in nursing facilities. Unnecessary hospitalizations of nursing facility residents are disruptive, disorienting, and often unsafe. Hospital care is also expensive. Medicare and Medicaid, the federally funded insurance programs that cover most long-term care costs, spend an estimated $1.9 billion each year on avoidable hospitalizations. Keeping nursing facility residents on site for care represents an opportunity to improve resident health, while reducing care costs.
Clinical and Educational Approaches to Reduce Both Avoidable Hospitalizations and Medicare Expenditures (NFI 1)
The Initiative to Reduce Avoidable Hospitalizations among Nursing Facility Residents (NFI)—a 2012-2016 Centers for Medicare & Medicaid Services (CMS) effort—tested a range of clinical care and educational interventions aimed at:
- Reducing avoidable hospitalizations among long-stay nursing facility residents
- Improving nursing home residents’ quality of care
- Decreasing health care costs.
The Initiative involved seven Enhanced Care and Coordination Provider (ECCP) organizations, partnering with about 150 nursing facilities across seven states. Interventions ranged from ECCP-provided education and training for facility staff to deployment of advanced practice registered nurses to provide resident assessments and care in participating facilities.
Financial Incentive Approaches to Reduce Both Avoidable Hospitalizations and Medicare Expenditures (NFI 2)
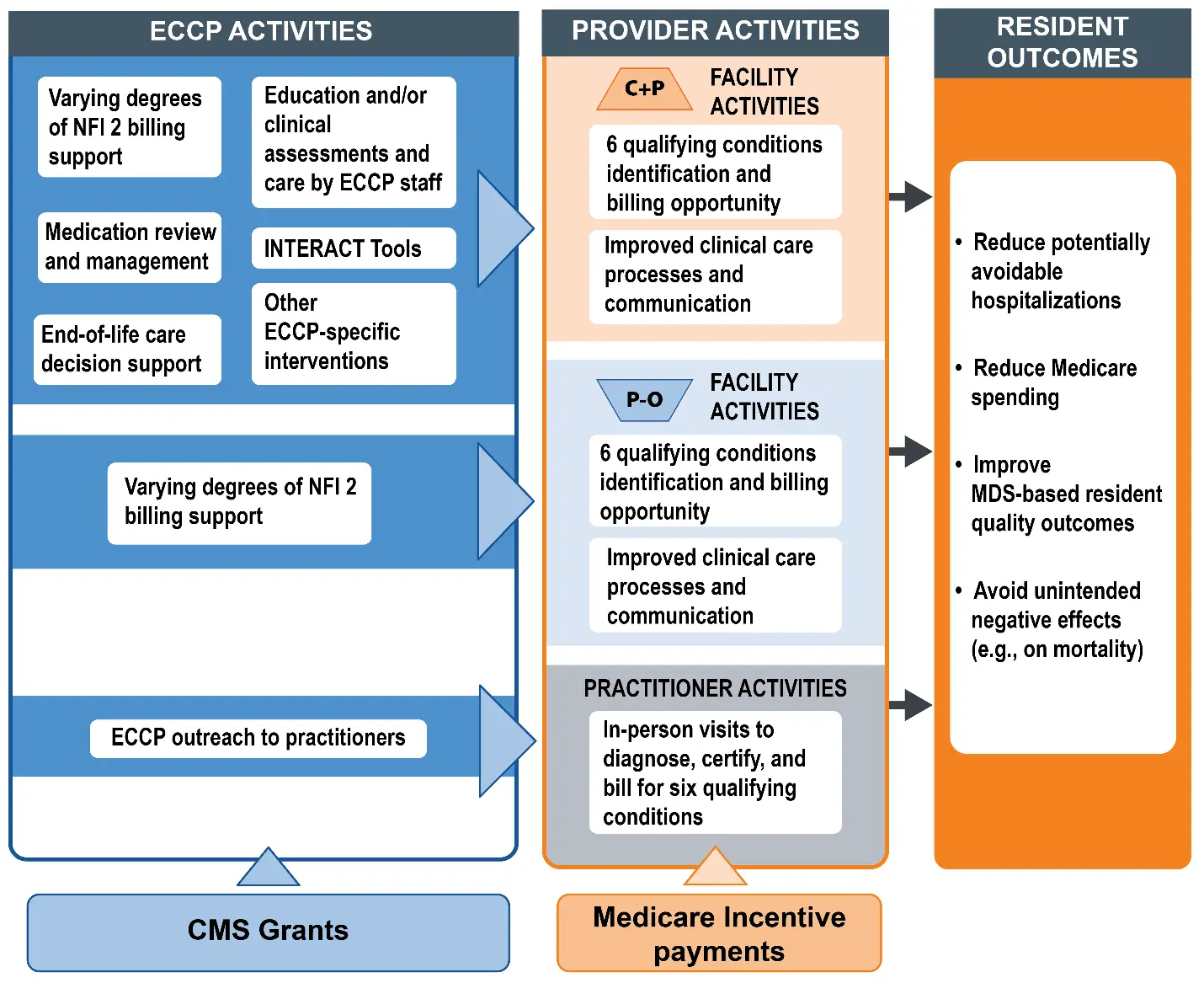
In 2016, CMS began implementing the second phase of the Initiative to Reduce Avoidable Hospitalizations among Nursing Facility Residents, adding a new Initiative-wide facility payment incentive and a second cohort of participating nursing facilities. This second phase of the Initiative concluded in October 2020. The model offered:
- Additional payments if the nursing facilities provided on-site care to residents with specific health conditions that commonly lead to hospitalizations.
- Facilities submitted Medicare claims for treating eligible residents on site, rather than transferring them to hospitals for care.
- Facilities could receive extra per diem payments for periods of in-house treatment.
- Additional payments to participating physicians and nurse practitioners for supporting facilities in this effort.
- Practitioners could bill Medicare Part B when evaluating residents for facility-based care.
- Practitioners could receive a hospital-level payment for this care.
The diagram below outlines the theory of action for NFI 2, highlighting how CMS intended the Initiative to be implemented and highlighting intended outcomes.
RTI’s Role in Helping Avoid Hospitalizations in Nursing Facility Residents
RTI’s team of national experts in program evaluation, Medicare payment policy, and health care for older adults, led the evaluation of both phases of the Initiative to Reduce Avoidable Hospitalizations among Nursing Facility Residents. Evaluation of Phase 2 is currently concluding.
Evaluation methods included extensive data analysis and multiple years of primary data collection. Implementation progress was assessed through site visits, telephone interviews, and surveys of participating facilities and affiliated practitioners.
Earlier research from RTI developed methods to identify avoidable hospitalizations in the nursing facility resident population, which served as a foundation for this work. To evaluate outcomes, RTI analyzed Medicare claims, nursing facility certification and survey data, and the Minimum Data Set. Key outcomes include hospital utilization, Medicare expenditures, and quality of care.
Key Finding: The support provided by Initiative hands-on advanced practice registered nurses in NFI 1 was associated with reductions in avoidable hospitalizations.
The RTI evaluation of NFI 1 found:
- Promising reductions in avoidable hospitalizations among eligible residents.
- Corresponding reductions in Medicare expenditures.
- No adverse impact on nursing home resident mortality.
- No effect on MDS-based quality outcomes.
RTI did not find net savings to the Medicare program after accounting for the costs of implementing NFI 1.
Key Finding: The evaluation found no clear evidence that the NFI 2 payment incentives were associated with favorable reductions in potentially avoidable hospitalizations and associated costs for eligible residents beyond what was achieved in NFI 1.
The RTI evaluation of NFI 2 found:
- No favorable impacts of the payment incentives alone on avoidable hospitalizations and corresponding Medicare expenditures among eligible residents.
- Simultaneously evaluating both NFI interventions together, the evaluation found that NFI 1 intervention had a favorable impact on reducing hospital-related utilization and associated expenditures and no clear evidence that the NFI 2 payment intervention had any additional positive effect beyond what was achieved in NFI 1.
- The COVID-19 pandemic had a devastating impact on residents and nursing facility staff, creating facility-wide operational challenges and impeding NFI 2 implementation in the final Initiative year.
Lasting Policy Impact of the RTI Evaluations
The first phase of this Initiative demonstrated the value of providing on site clinical support for nursing facilities, which are generally understaffed and struggle with recruiting and retaining direct care and nursing staff. The second phase highlighted the challenges of developing and structuring sufficient and appropriate financial incentives to change provider behavior.