Comparing Lovo-Cel Gene Therapy to Common Sickle Cell Disease Treatment
Objective
To develop an economic model to predict the cost-effectiveness of lovo-cel, a recently approved gene therapy, for patients living with sickle cell disease (SCD) and experiencing recurrent vaso-occlusive events in the United States.
Approach
Using evidence from lovo-cel clinical trials and the published literature, we predicted the lifetime benefits, costs, and cost-effectiveness (or value for money) of lovo-cel in comparison with common care for patients with SCD.
Impact
Our study predicted meaningful improvements in survival, quality of life, and other health outcomes for patients treated with lovo-cel. Our analysis also highlighted the contribution of predicted patient productivity gains and reduced caregiver burden to the potential societal value of gene therapy for SCD. These findings will help inform patients, clinicians, and families considering treatment options for SCD.
What is Sickle Cell Disease and Who Does it Affect?
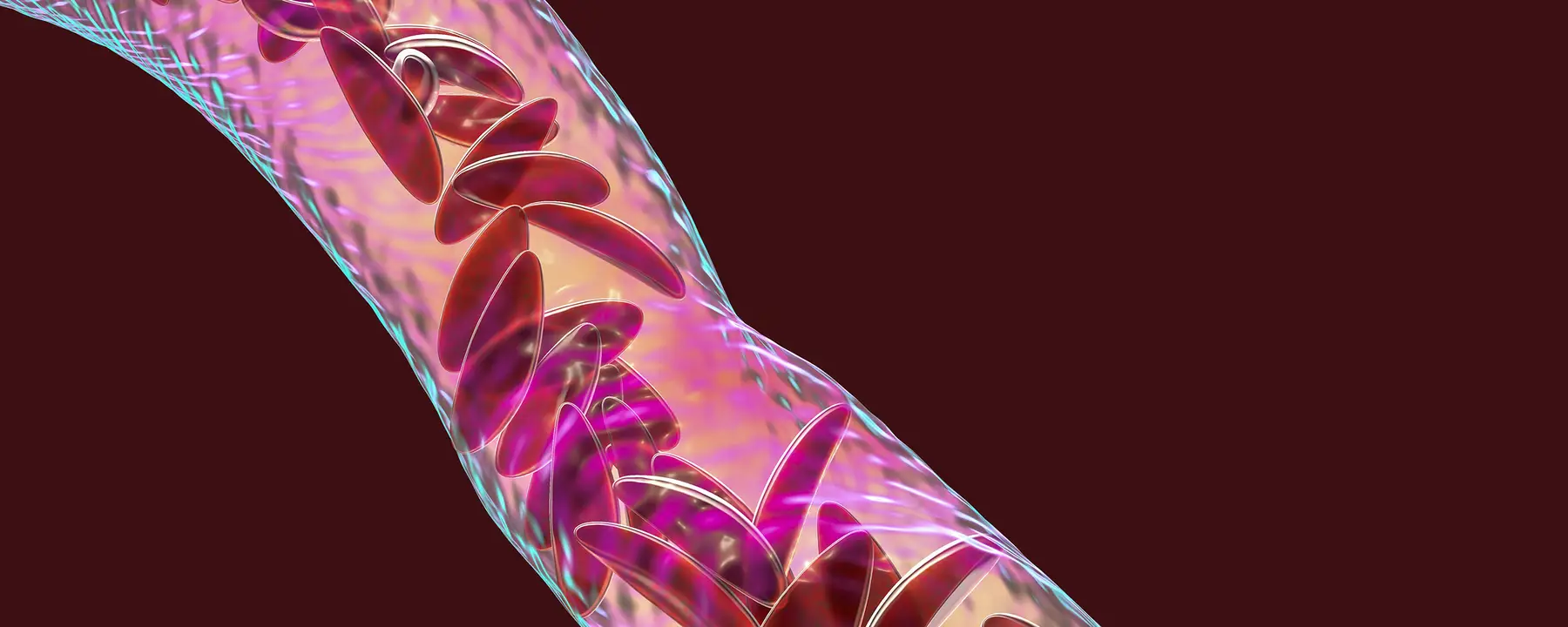
Sickle cell disease (SCD) is a rare hereditary blood disorder that causes red blood cells to contort into a sickle or crescent shape. These cells die earlier than normal red blood cells, impairing blood flow and oxygen delivery to the body. This impairment can lead to anemia and blood vessel obstruction. When sickled cells block blood circulation, those with SCD often experience painful and debilitating complications known as vaso-occlusive events.
Vaso-occlusive events are life threatening, causing extreme pain, stokes, jaundice, organ damage, and in worst cases, death. Over time, individuals with SCD also are at increased risk of stroke and multisystem organ damage. Consequently, people living with SCD have a life span cut short by several decades. The life expectancy of approximately 100,000 people living with SCD in the United States (US) is estimated to be 52 years, with more severe variations of the disease having a life expectancy closer to 40 years.
Current Treatments for Sickle Cell Disease
While treatments exist to alleviate symptoms, better options are needed to decrease vaso-occlusive events and extend life expectancy for people living with SCD. Current SCD management includes chronic and acute therapies like opioid and nonopioid pain management, red blood cell transfusions, hydration therapy, and hydroxyurea. Use of newer disease-modifying therapies remains limited. A potential cure based on stem cell transplantation exists, but very few patients are eligible for it. This option, known as allogenic hematopoietic stem cell transplantation, is only available for the small proportion of individuals with a suitable and willing human leukocyte antigen-matched sibling donor.
New Gene Therapy Treatment for Sickle Cell Disease
In 2023, the US Food and Drug Administration approved lovotibeglogene autotemcel (lovo-cel), a new one-time gene therapy for SCD administered via autologous hematopoietic stem cell transplantation. In this type of transplantation, a patient’s own stem cells are collected, modified, and returned to the patient. The modified cells with lovo-cel produce anti-sickling hemoglobin, resulting in complete resolution of vaso-occlusive events for 88% of those treated in clinical trials. While treatment with lovo-cel offers potentially curative benefits for patients with SCD, little is known about its long-term effectiveness, prompting important discussions about value, access, and affordability.
RTI Health Solutions’ Cost-Effectiveness Analysis for Lovo-Cel
To investigate the potential clinical and economic benefits of lovo-cel, RTI Health Solutions researchers developed a lifetime economic model to predict the cost-effectiveness (or value for money) of lovo-cel for patients living with SCD and experiencing reoccurring vaso-occlusive events from a societal perspective in the US. In addition to relying on evidence from lovo-cel clinical trials and the published literature, we sought the expertise of clinical and economic advisors and a patient with SCD when developing the model.
Our analysis predicted a meaningful increase in life expectancy for patients treated with lovo-cel compared with common care, driven in part by reductions in vaso-occlusive events and other SCD-related complications. These clinical benefits were accompanied by predicted improvements in patients’ quality of life, gains in educational and productivity outcomes, and reductions in caregiver burden. The high one-time cost of lovo-cel gene therapy was partially offset by predicted reductions in the medical costs associated with common care and SCD-related complications. Overall, lovo-cel was predicted to be cost-effective compared with common care at US society’s typical willingness-to-pay levels for health gains. The predicted societal value of lovo-cel was found to be most sensitive to patients’ age and severity at the time of treatment and to the durability of the lovo-cel treatment effect.
We compared the cost associated with lovo-cel with common SCD treatments, particularly the offset of cost for common treatments to mitigate SCD side effects. Our report found an overwhelmingly positive impact from lovo-cel. On average, patients experienced an increase in productivity, relying less on caregivers. The cost-effectiveness of lovo-cel proved to be depended on a patient’s severity of SCD and their age. For example, lovo-cel cannot reverse existing vascular damage. SCD patients who were younger and received lovo-cel experienced a great reduction in vaso-occlusive events.
Additionally, we found that lovo-cel drastically increased the life expectancy of people with SCD compared to common care. Patients on common care were predicted on average to survive 13.47 years, experience 3.94 cumulative chronic complications, and 67.81 lifetime vaso-occlusive events per patient. In comparison, patients treated with lovo-cel were predicted to survive 37.32 years, experience 2.05 cumulative chronic complications, and 6.75 lifetime vaso-occlusive events per patient.
Lovo-cel’s Potential for Sickle Cell Disease
Our study sought to quantify the potentially meaningful improvements in lifetime health and economic trajectories for patients with SCD with recurring vaso-occlusive events treated with lovo-cel in comparison with common care. Although uncertainty remains about the long-term curative potential of lovo-cel gene therapy, these findings can facilitate open dialogue and shared decision-making among patients, families, and healthcare providers considering lovo-cel as a treatment option for SCD in the United States.
- bluebird bio