CMS Health Equity Conference
Date
Location
United States
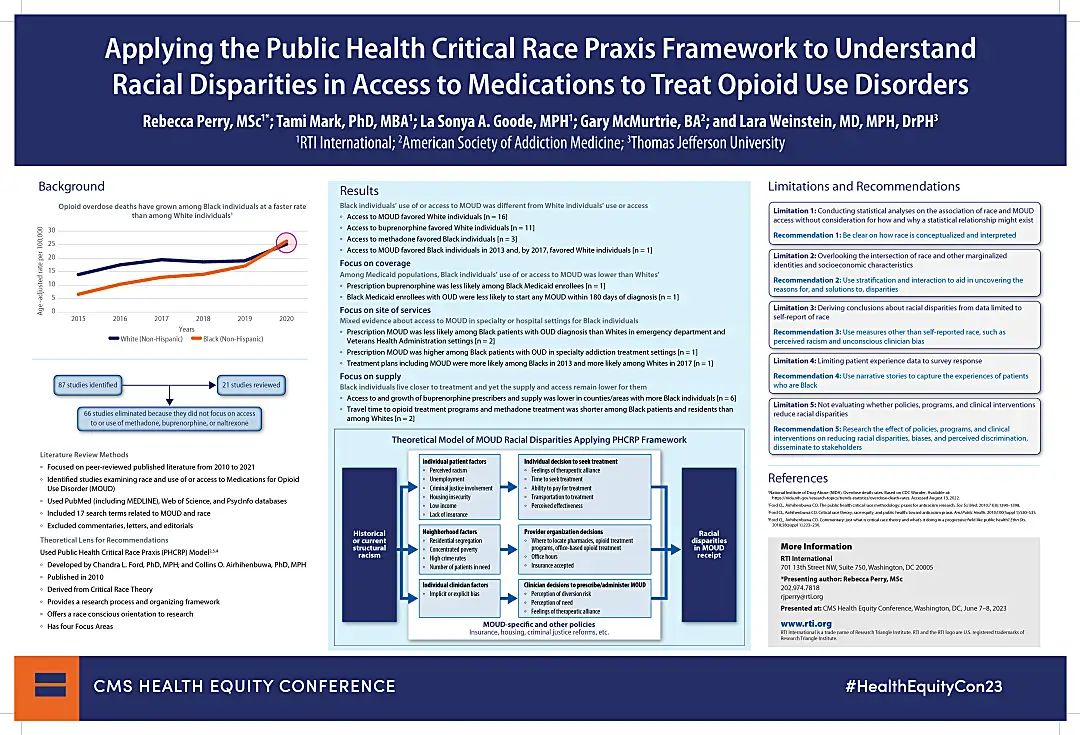
From 2010 to 2020, the opioid overdose death rate among Black individuals rose 4 times faster than the rate among White individuals over that period. In 2020 only, overdose death rates for Black individuals increased 44 percent compared to the previous year and were 50% higher than White individuals. To understand these disparate outcomes, health equity scholars recommend examining the structural factors that serve as a driver. Join us at the CMS Health Equity Conference to learn about racial disparities in access to and use of Medications for Opioid Use Disorder (MOUD).
Applying the Public Health Critical Race Praxis Framework to Understand Racial Disparities in Access to Medications to Treat Opioid Use Disorders
Racial disparities in access to care are ubiquitous in the US healthcare system. Health equity scholars have recommended attention to theoretical frameworks that highlight the structural underpinnings of disparities. The Public Health Critical Race Praxis (PHCRP) is a structural-focused racial disparities framework that presents four focus areas for conducting research on race:
- Conceptualize the mechanisms of structural racism in operation during the study's period.
- Explore how methods and interpretations of findings may be biased in preconceived assumptions and bring in the voice of Black patients.
- Acknowledge the intersection of race and other socioeconomic factors and marginalized identities.
- Use the research to disrupt causes of inequities, not just document them.
RTI Public Health Analyst, Rebecca Perry, will review the findings of a literature review focused on MOUD and share practical recommendations that use the theoretical framework of PHCRP to help future researchers, policymakers and program developers move beyond simply identifying racial disparities and move toward reducing them.

Rebecca J. Perry, Public Health Analyst
Rebecca Perry has over 15 years of applied and research experience centered around health care coverage and access for underserved populations, including tribal and native American populations, Medicaid and uninsured individuals, and individuals with behavioral health disorders.


